LONDON, ONT. -- It was an attempt to get her help. Cathy Johnston's family called an ambulance after Cathy, who suffers from dementia, repeatedly wandered away from her home. It's a decision they regret.
“I would not have called the ambulance if I knew that was what they were going to do to her. Lock her down there,” says her husband Jack Johnston.
Jack is referring to the seclusion rooms within Victoria Hospital's emergency department.
Seclusion rooms are often used as a temporary space for severe mental health patients, and it’s where 67-year-old Cathy was placed for almost a week.
“I saw the room and I said, 'This is not right for her, like is going to drive her crazy being in a room like that,'” says Jack.
There are four seclusion rooms in the emergency department at the London Health Sciences Centre's (LHSC) Victoria Hospital campus.
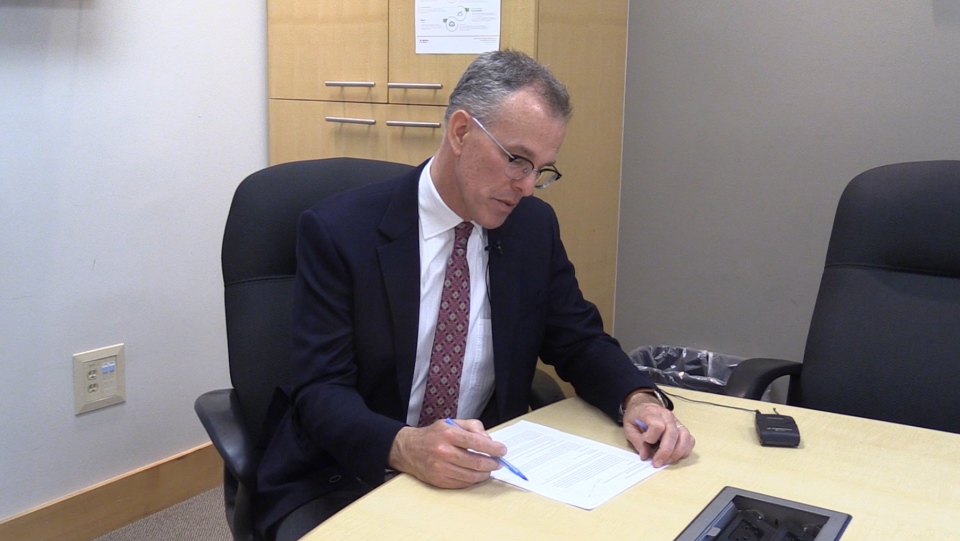
“Seclusion rooms are specific to patients who are experiencing behavioral crisis due to, usually, their mental health,” says Tom McHugh, vice president of Mental Health at LHSC.
McHugh says sometimes seclusion rooms are used because other, more suited rooms aren’t available to patients.
“They are used as quiet spaces, but they aren’t designed for long-stay patients at all.” When asked what qualified as a long-stay though, McHugh wouldn’t say.
Cathy Johnston stayed in the seclusion area for six days.
McHugh says, “We do apologize to this family and patient that we have not met their expectations."
Cathy’s sister Cindy Fitzsimons says the damage has already been done.
“I’m in shock but I’m also disgusted at our health care,” she says. “When you go to an emergency room you expect to get the care you need not get treated like that.”
The family also reached out to London West MPP Peggy Sattler about the situation. Sattler believes provincial cuts to health care will only make situations like these worse
“We have to make sure that people keep getting the kind of care and quality of care they deserve,” says Sattler. “Why? Why do we see this happening over and over again?”
The hospital maintains patient care is the top priority, and it's always striving to do better.
“I would love to see us right-size, to be able to see a patient in [emergency], make the designation that would make them benefit from an inpatient stay and get them right up to the unit,” says McHugh.
But he adds, “That’s in a context of an upstream and downstream capacity as well, all of which are stretched currently in Ontario.”
After six days in the seclusion area, Cathy was moved to a secure mental health ward, and then Tuesday night she was moved into a Geriatrics Unit that specializes in dementia care.
In part three of our continuing coverage, we will look at how that move has now affected another dementia patient within the hospital.