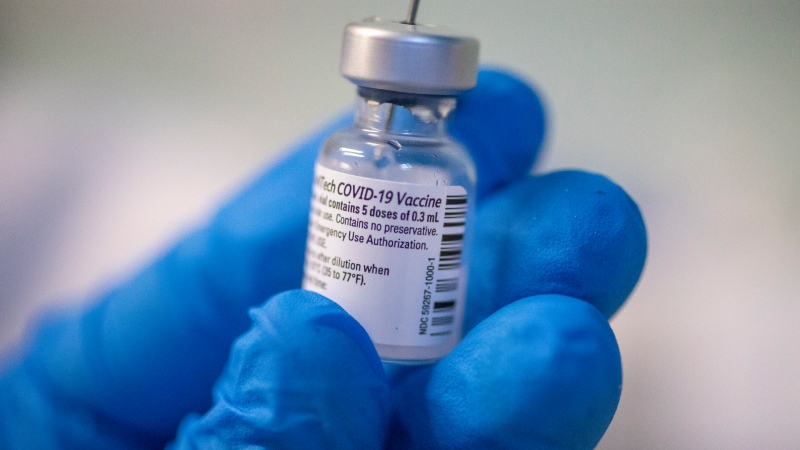
LONDON, ONT. -- Doctors aren't panicking over the coronavirus and said you shouldn't either, says a local public health expert.
“The biggest risk with COVID-19 is panicking,” said Dr. Chris Mackie, CEO of the Middlesex-London Health Unit, via Twitter.
The risk to those in the Middlesex County and London remains low.
But even with that being said, Canada’s chief public health officer has stressed the importance of preparedness in the event it becomes a pandemic.
Mackie understands that coronavirus is a big deal but says, “It’s a big deal that we have spent many years preparing for.”
Mackie was in medical school when the world experienced an outbreak of SARS (Severe Acute Respiratory Syndrome) in 2002.
He says that virtually everyone working in public health across Canada either grew up or has worked in a post-SARS era.
“We think about this all the time,” he tweeted, “We plan for it. We train for it. We hope it never comes, but when it does, we are ready.”
Mackie explains that initially the SARS illness seemed to be linked with travel to China, but that the Chinese government was not saying anything about it. Because of this, it took months to develop a lab test to confirm the illness and the results were very slow.
He calls the situation with COVID-19 “much different.”
With COVID-19, lab tests were made available almost immediately using PCR (Polymerase chain reaction) technology.
Doctors can now identify coronavirus through throat swabs and it can be detected within days of the illness beginning, not weeks.
“The lab tests that were quickly developed for COVID-19 use PCR technology, which only needs a tiny fragment of DNA to identify a case,” he tweeted. “PCR testing is generally very accurate.”
Health care workers are also prepared for the coronavirus. Seventeen years ago with SARS, high-risk procedures were performed in crowded emergency rooms.
Procedures like a bronchoscopy, which is the insertion of a tiny camera on the end of a probe into a patient's lungs, and can cause coughing and propel the virus.
Now a bronchoscopy is never done in crowded areas but only in controlled conditions, he said.
Isolation is a key factor in containing the virus. The vast majority of cases of COVID-19 in Canada are being isolated at home instead of being in a health care setting.
Mackie says that locally, we have had regular contact between health care organizations and municipalities in addressing outbreaks - and the province now has Public Health Ontario, an organization tasked with monitoring COVID-19.
When issues like COVID-19 occur, the MLHU notifies over 1,000 health care leaders across London and Middlesex County.