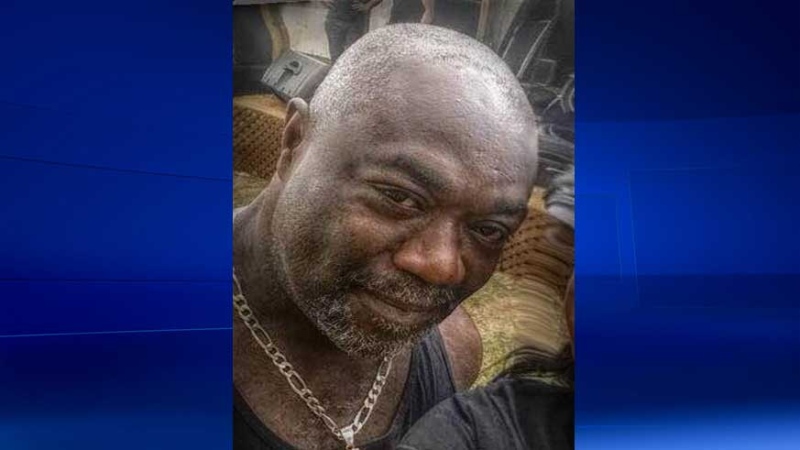
LONDON, ONT. -- "I miss him so much."
It’s been seven years since Marilyn Reid last saw and spoke to her husband John. It was in February of 2013 that he was brought to Victoria Hospital via ambulance, suicidal and in crisis.
“When we got him there I was very relieved and I thought he was safe and in good hands.”
John, a veteran of the Canadian Armed Forces suffered from post-traumatic stress disorder (PTSD) and was having suicidal thoughts.
“He was in the hospital in crisis and was there a week in crisis and then was released, but nobody contacted me to tell me that he was leaving the hospital. I was actually in shock.”
Reid says she received a phone call from the hospital, one that forever changed her life.
“The only phone call I got from them was to tell me that he was deceased and that he died on hospital grounds. He took his life, just very shortly after they released him.”
Reid says after seeing the CTV News story last week about a suicidal woman going missing after being discharged from Victoria Hospital, she knew she had to speak out.
“I cant believe that people are being released from the hospital and their loved ones aren’t being contacted. It’s been a few years since my husband died and I can’t believe this is still going on.”
The London Health Coalition believes the care for mental health patients is only going to get worse if there continues to be a lack of services and funding for mental health care.
“We in this community have already suffered from losing so many beds, thousands literally,” says Peter Bergmanis from the London Health Coalition. “There was the London Psychiatric Hospital and the St. Thomas Psychiatric Hospital that are vacant. So where are these people supposed to go?”
Reid agrees more funding and services would be key, but in the interim would like to see hospitals contacting family before discharging mental health patients.
“I, in my heart feel if I could have seen him and talked to him again that the outcome would’ve been entirely different.”
Policies differ from hospital hospital when it comes to notifying family of patient discharge.
In a statement the London Health Sciences Centre said, “Our care providers work with patients to support their discharge, including calling their families/supports when needed. We welcome families sharing their concerns with us, and we are committed to working with them directly.”
Meanwhile St. Thomas Elgin General Hospital states, “When a patient presents in the Emergency Department, they are triaged by a nurse and assessed by a skilled emergency physician. Based on the assessment, a decision to admit or discharge would be made. The decision to notify a family member is determined through a conversation with the patient. This process remains unchanged during COVID.“