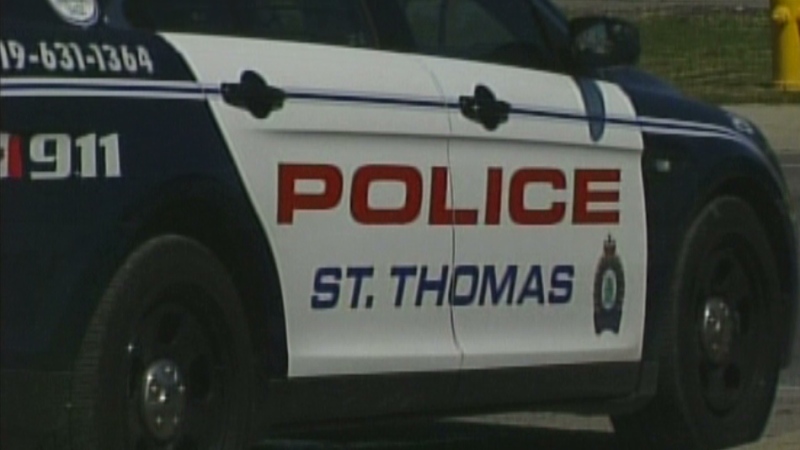
An average London police officer spends three quarters of their day on duties unrelated to crime - including paperwork or dealing with mental health patients.
Since the 1960s, mental health treatments have been increasingly de-institutionalized and without adequate community supports, those in crisis rely on emergency services - pushing first responders into a near crisis of their own.
The London Police Service has introduced programs and partnerships to help ease the pressure on its services, but mental health calls - best handled by the medical community - still account for about 15 per cent of its entire budget.
During one shift, Sgt. Marcel Marcellin says, "We might get three, four or even five calls from individuals suffering from mental health problems."
And when that happens, police, EMS and hospitals are all involved.
Police cars can often be seen lined up outside the London Health Sciences Centre, waiting to transfer custody to the hospital and ensure they - and other patients - are safe.
All those cars in the hospital parking lot means fewer officers on the street.
Marcellin says, "If we have several officers down here in that transition period, it has a strain on our resources for calls for service."
And it's a big strain. London police estimate they handled over 2,000 mental health calls in 2014 - calls that may have been better dealt with in the medical community.
Chief Brad Duncan says, "In the past 10 or 12 years, we've seen a real increase in the number of individuals that we're dealing with on a regular basis. And some of that, I think, is attributable to the de-institutionalization of mental health.
"And so individuals are moved from a health care facility onto the street and I think initially that was positive in that people don't have to be housed in an institution, however, the framework wasn't there and so many of these individuals fell through the cracks."
The framework needed? Better community mental health services.
London often trails other cities when in comes to mental health services. The average wait for funded counselling and treatment is nearly two months, making the South West LHIN 11th out of 14 in terms of wait times.
Average Counselling and Treatment Wait Times By LHIN (Local Health Integration Network) in Third Quarter of 2014
- North West - 7 days
- Central East - 20 days
- Waterloo Wellington - 23 days
- Erie St. Clair - 29 days
- Mississauga Halton - 30 days
- South East - 36 days
- North Simcoe Muskoka - 41 days
- North East - 42 days
- Central - 50 days
- Central West - 50 days
- South West - 58 days
- Hamilton Niagara Haldimand Brant - 60 days
- Toronto Central - 91 days
- Champlain - 106 days
It's these types of services that could prevent situations where an individual in distress or crisis ends up in a confrontation with police, requiring the response of dozens of officers and hours of time, when a health care intervention is what was really needed.
Duncan adds, "If we do nothing to avert this, then the dollars spent by 2015 will be in the neighbourhood of $16 million out of a nearly hundred-million dollar budget. That's significant."
Case Management Wait Times By LHIN (Local Health Integration Network) in Third Quarter of 2014
- North West - 7 days
- North East - 20 days
- Central East - 20 days
- Erie- St. Clair - 22 days
- Hamilton Niagara Haldimand Brant - 26 days
- Mississauga Halton - 28 days
- South East - 29 days
- South West - 30 days
- Toronto Central - 47 days
- Central - 53 days
- Champlain - 68 days
- North Simcoe Muskoka - 69 days
- Waterloo Wellington - 101 days
- Central West - 127 days
Coming up in part two: Police have developed new partnerships with the Canadian Mental Health Association which are helping to relieve some of the strain, but it's a work in progress for them and other emerency services.